Medicare Eligibility Requirements for 2020
Not sure if you’re eligible for Medicare health insurance? The Social Security Administration (SSA) enrolls some people automatically. But don’t expect that or wait for your Medicare card to show up. Find out if you’re eligible now so you can enroll at the right time and avoid any Late Enrollment Penalties (LEPs).
There’s more than one way to qualify for Medicare, and enrolling in the different parts of Medicare differ as well. Plus, how you qualify may determine how you can receive coverage and what your premiums might be.
If you’re looking for more of a crash course in the different parts of Medicare and how the program works as a whole, check out our Ultimate Medicare Guide. Otherwise, read on.
Medicare eligibility requirements - Part A and Part B
The Centers for Medicare & Medicaid Services (CMS) runs the Medicare program, but it doesn’t determine who’s eligible. That job falls on the Social Security Administration (SSA). Newly eligible enrollees apply for benefits through the Social Security Administration.
People qualify for Medicare health insurance in one of three ways:
- Age 65 or older
- Disability - those who have been receiving disability benefits for at least 24 months
- Illnesses such as end-stage renal disease (ESRD) or amyotrophic lateral sclerosis (ALS)
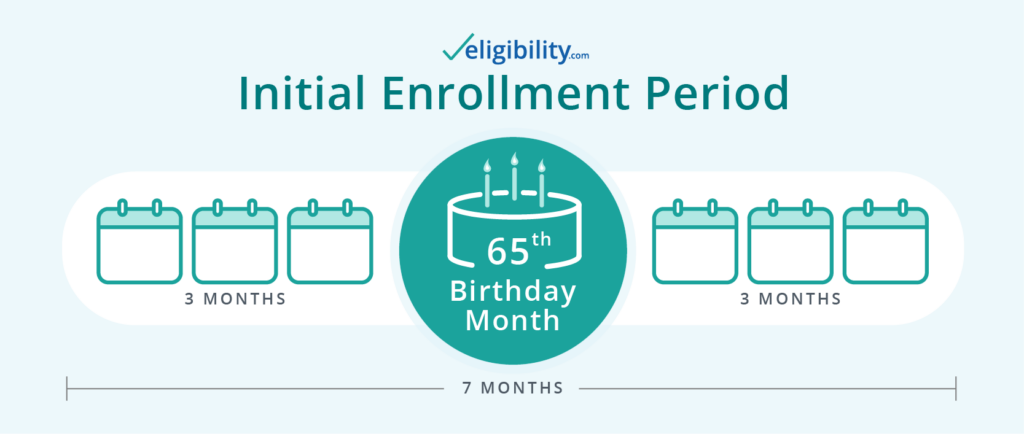
If you already receive Social Security or Railroad Retirement Board (RRB) benefits when you gain eligibility for Medicare health insurance, Uncle Sam may automatically enroll you. Otherwise, you'll likely use your Initial Enrollment Period (IEP), a seven-month window that begins three months before you become eligible for coverage.
Learn more about when and how to apply for Medicare.
Those who become eligible for Medicare at age 65 in 2020 won't be eligible for full Social Security retirement benefits for another 14 months.1 If you start taking your benefits before turning 65, however, you may be auto-enrolled in Medicare.
Medicare eligibility age
The majority of people first join the ranks of Medicare beneficiaries the month they turn 65. If you qualify for Medicare this way, your Initial Enrollment Period will begin three months before the month you turn 65.
Medicare eligibility by disability
Most Medicare recipients under the age of 65 reach eligibility during their 25th month receiving Social Security disability benefits. If you qualify for Medicare because of a disability, your Initial Enrollment Period will begin during the 22nd month you receive these benefits—three months before you’re eligible for coverage.

Medicare eligibility due to specific illnesses
In addition to the above ways to qualify for Medicare health insurance, you may also be eligible if you have one of the following diseases:
- End-stage renal disease. To qualify, you must need regular dialysis or a kidney transplant, and your coverage can begin shortly after your first dialysis treatment. If you receive a transplant and no longer require dialysis, you’ll lose Medicare eligibility.
- Amyotrophic lateral sclerosis. Also known as Lou Gehrig’s Disease, patients diagnosed with this terminal disease gain immediate Medicare eligibility.
Can I apply for Medicare at age 62 or do I have to be 65?
Although you may be able to begin withdrawing Social Security benefits for retirement at age 62, Medicare isn't available to most people until they turn 65. But if you are under the age of 65, you could be eligible for Medicare if you meet any of the following criteria.
- You have been receiving Social Security disability benefits for at least 24 months.
- You receive a disability pension from the Railroad Retirement Board and meet certain criteria.
- You have Lou Gehrig’s disease (ALS).
- You have ESRD requiring regular dialysis or a kidney transplant, and you or your spouse has paid Social Security taxes for a length of time that depends on your age.
If none of these situations apply to you, you'll have to wait until age 65 to begin receiving your Medicare benefits. However, you can begin the sign-up process three months before the month you turn 65 during your IEP (discussed above).
Requalifying for Medicare at 65
If you become eligible for Medicare before you turn 65 due to disability or one of the above diagnoses, you’ll requalify again when you reach age 65. When you do, you’ll have another Initial Enrollment Period and all the benefits of a newly eligible Medicare recipient, such as a Medicare Supplement Enrollment Period.
Medicare Advantage (Part C) eligibility
Medicare Advantage is an alternative to Original Medicare. Private companies provide Medicare-approved plans that cover everything Original Medicare covers, as well as additional benefits that may include vision, dental, hearing, and prescription drug coverage.
To be eligible for Medicare Advantage, you must meet the following requirements:
- You must be eligible for both Part A and Part B (original Medicare).
- You must live where plans are available.
- You can't have end stage renal disease (unless enrolling in a plan tailored to ESRD patients).
- You must pay Part A, Part B, and Medicare Advantage premiums, if applicable.
If you meet these requirements, learn why you might choose Original Medicare or Medicare Advantage.
Medicare Supplement eligibility
Also known as Medigap, Medicare Supplement plans are designed to accompany Original Medicare. They help cover additional Part A and Part B costs, such as deductibles and copayments.
To be eligible for a Medicare Supplement plan, you'll need to meet the following requirements:
- You must have both Part A and B (original Medicare).
- You must live where plans are available.
- You must pay Part A, Part B, and Medicare Supplement premiums, if applicable.
Medicare Part D prescription drug coverage eligibility
Like Medicare Advantage and Medicare Supplement, Part D prescription drug coverage is provided by Medicare-approved private insurance companies. These plans accompany Original Medicare. Generally, you can’t have a standalone Part D plan if you have a Medicare Advantage plan.
To qualify for a Part D plan, you must meet the following requirements:
- You must have both Part A and B (original Medicare).
- You must live where plans are available.
- You must pay Part A, Part B, and Part D premiums, if applicable.
Additional Medicare requirements
We’ve gone over the ways people become eligible for Medicare, Medicare Advantage, Medicare Part D prescription drug coverage, and Medicare Supplement plans. We have also covered how to qualify for the various parts of Medicare. But you’ll need to meet additional requirements as well, including the following:
- You will need to be a US citizen or have been a legal resident for at least five years.
- You can’t be imprisoned in a correctional facility.
- You must have a stable US address, even if you spend your days RVing around the nation.
- In most cases, you’ll need to receive care within the US, not abroad.
- You can't contribute to a Health Savings Account (HSA), though you can still use existing funds in your account.
If you’re newly eligible, it’s also a smart idea to learn how to get started with Medicare.
Medicare, other insurance, and how we can help
Did you know you can enroll in Medicare even if you have other kinds of insurance such as Medicaid, VA benefits, and employer-sponsored health insurance? That said, some of these types of insurance work better with Medicare than others. In some cases, they may affect your ability to enroll in Medicare.
To find out how to choose the right Medicare coverage and understand how it will interact with health insurance you may already have, call the number below. A licensed Medicare expert can answer your Medicare eligibility questions—and help you enroll.
1. Social Security Administration, "Benefits Planner: Retirement"
2. Medicare, “Part B Costs”
Content on this site has not been reviewed or endorsed by the Centers for Medicare & Medicaid Services, the United States Government, any state Medicare agency, or any private insurance agency (collectively "Medicare System Providers"). Eligibility.com is a DBA of Clear Link Technologies, LLC and is not affiliated with any Medicare System Providers.



