Medicare and Home Health Care
If you need skilled nursing care, some kinds of therapy, hospice, or other services in your home, Medicare may cover those home health services. If you need custodial care, however, Medicare probably won't pay for it.
Read on to find out how much Medicare will pay for, how to qualify for home health care coverage, and what to do if the services you need aren't covered.
Home health care could be a key part of social distancing for Medicare beneficiaries. Receiving medical care at home can prevent the spread of coronavirus and free up hospital bed for critical patients.
Ask your home health care provider about the precautions their workers are taking to guard against COVID-19 and protect their workers and patients.
What home health care services does Medicare cover?
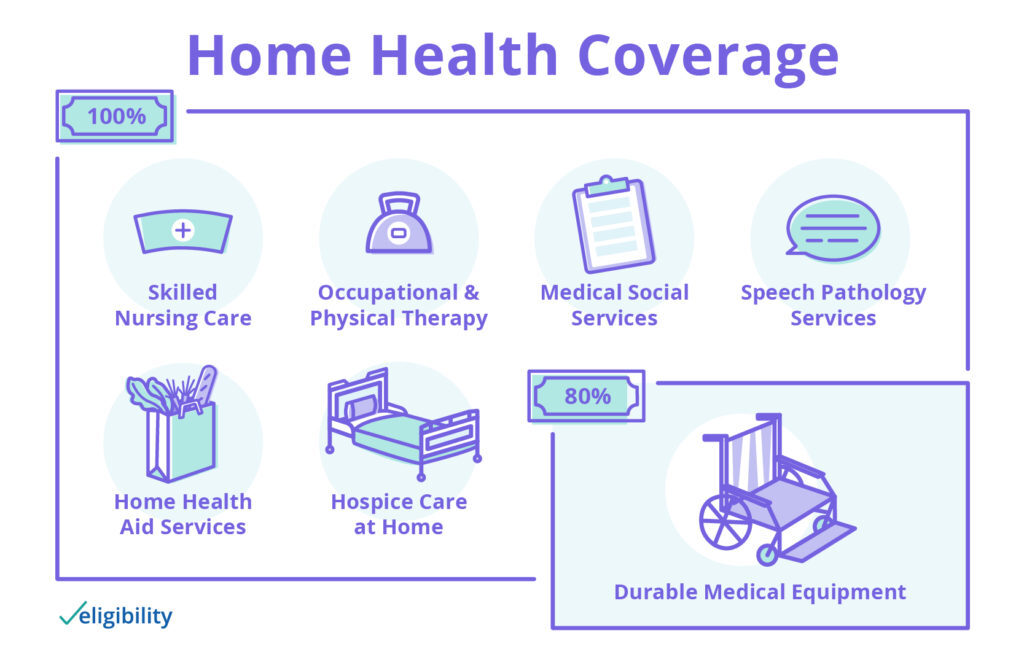
Medicare covers home health services, such as the following:
- Skilled nursing care (part-time or intermittent)
- Occupational and physical therapy
- Medical social services
- Speech-language pathology services
- Home health aide services (part-time or intermittent)
- Hospice care at home
For the above services, Original Medicare (Parts A and B) will cover 100% of your costs for home health care service. If you need durable medical equipment for use with home health care, Medicare will cover 80% of the price.
Some home health services are covered under Part A, while others are covered by Part B. Learn more about these parts of Medicare with our Guide to Medicare.
If you have Medicare Advantage, your plan may cover more home health services under specific conditions. Learn more about the additional home health and other benefits many Medicare Advantage plans have added in 2020.
How can I qualify for Medicare home health care?
Home health care is designed for people who can’t make it to the doctor very often because they’re homebound. That means your regular doctor (usually a primary care physician, also known as a PCP) must certify that you have difficulty leaving home. Your doctor must also confirm that you need one or more of the covered services listed above.
Medicare home health care coverage may not be enough for people who need long-term care at home. If you require home health care for more than eight hours a day or for seven days per week, you’ll have to pay out of pocket.
To receive Medicare home health care coverage, you must have both Part A and Part B. If you don’t have them, find out if you’re eligible for Medicare.
If you have Medicare Advantage, you’ll receive the same home health care coverage that Parts A and B pay for. You may also receive other benefits such as Medicare prescription drug coverage and dental care. Learn more about Medicare Advantage plans.
What home health care services doesn’t Medicare cover?
There are limits to what Medicare typically covers when it comes to home health care. It probably won't include the following services:
- 24-hour home care
- Meal delivery services (such as Meals On Wheels)
- Homemaking or housekeeping services
Does Medicare cover custodial care?
Medicare may not pay for personal or custodial care, which includes the six activities of daily living: toileting, bathing, eating, dressing, transferring, and continence. Medicare will cover these services only if you also need other covered home health care services, and only if you need part-time care.
How can I receive health care coverage with Medicare?
To receive home health care Medicare benefits, you must receive covered services from qualified health professionals. Additionally, all home health care under Medicare must be administered by a Medicare-certified home health agency.
Any services you receive require pre-approval by your home health agency. If you need a service Medicare doesn't cover or that's only partially covered, you will receive written notice that you’ll need to cover some or all of the cost before using those services.
What if Medicare doesn’t cover my home health care needs?
If you need home healthcare services, Medicare may pay for some or all of these expenses. If you require services Medicare doesn’t cover, you have options.
Your state Medicaid program may be able to help. Many Medicaid programs cover services Medicare doesn’t, so check your state’s program for details.
Alternatively, Original Medicare beneficiaries can switch to a Medicare Advantage plan during Medicare Open Enrollment. You could find a plan that covers more services than Original Medicare.
And we can help. Call a licensed sales agent to learn what plans are available in your area and whether they can help minimize your health care expenses.
Have more Medicare questions?
- Does Medicare cover assisted living?
- Does Medicare cover vision care?
- Does Medicare cover dental care?
- What are other Medicare costs I need to know about?
Content on this site has not been reviewed or endorsed by the Centers for Medicare & Medicaid Services, the United States Government, any state Medicare agency, or any private insurance agency (collectively "Medicare System Providers"). Eligibility.com is a DBA of Clear Link Technologies, LLC and is not affiliated with any Medicare System Providers.



